Course in treatment 4/27/2017 treatment plan treatment plan for kelly nesmith a treatment plan was created or reviewed today, 4/27/2017, for kelly nesmith. He didn’t have any physical limitations. Page 5 of 7 time spent face to face with patient and/or family and coordination of care: Join thousands of happy therapists using mentalyc ai. Abe was taking vasotec, 10 mg, 2x per day with full adherence to treat high blood.
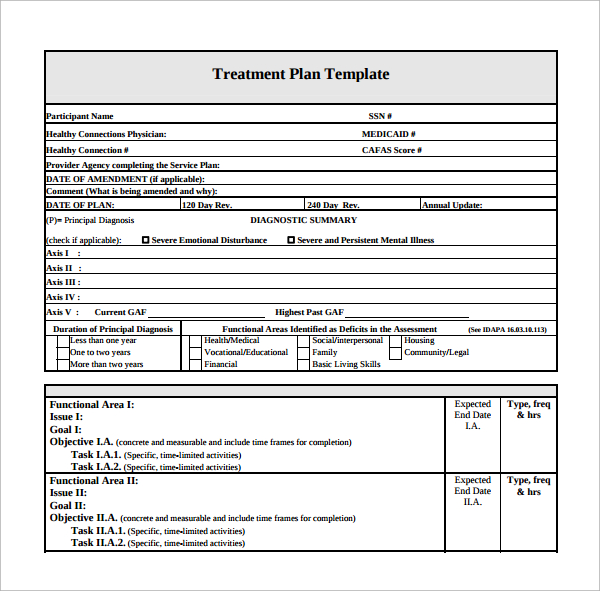
What is a treatment plan? Web a treatment plan template is a standardized document that outlines the goals, strategies, and interventions for a client’s mental health treatment. Look at how the barrier or need impacts the client’s life, not just that it exists and is impacting them. At the most basic level, a mental health treatment plan is simply a set of written instructions and records relating to the treatment of.
Web a treatment plan template is a standardized document that outlines the goals, strategies, and interventions for a client’s mental health treatment. In psychology and related fields, a case conceptualization summarizes the key facts and findings from an evaluation to provide. Psychological therapies for people with severe mental health problems (also referred to as severe mental illness) are a key part of the new integrated offer for adults and older adults, as set out in the nhs long term plan (ltp) and the community mental health framework for adults and older adults.severe mental health.
Mental Health Care Plan Template 9+ Free Sample, Example, Format Download
Join thousands of happy therapists using mentalyc ai. Web this document is a template of a mental health treatment plan. Progress notes are the core piece of documentation a mental health care provider should write after each session with a client, but it’s more than just a record of what happened in the session. What is a treatment plan? Progress notes keep a record of the client's progress and the care you provide.
What is a case conceptualization or formulation? Web become a headway provider. Progress notes keep a record of the client's progress and the care you provide.
You're Not Alone If You're A Therapist Who Feels Utterly Lost When Writing A New Client's Biopsychosocial (Bps) Assessment.
Carepatron offers a standardized format for documenting client sessions and treatment progress, ensuring consistency across all client records. It serves as a guide for both the therapist and the client, providing a structured plan to address the client’s specific needs and concerns. Try it out for free. The discharge process is a critical component of overall treatment management in mental health care.
His Health Was Relatively Good, Except For Moderately High Blood Pressure, Which He Developed In His Late Forties.
Whether you are beginning your wellness journey or guiding clients through theirs, dive in to discover how you can take control and shape the narrative of health, healing, and hope. Specify where the client’s behavioral health symptoms and life. Page 5 of 7 time spent face to face with patient and/or family and coordination of care: (consider how symptoms/functional impairments or other factors/issues may be interfering with recovery progress.
It Details The Client's Condition, Symptoms, Diagnoses, Interventions, Outcomes, And Recommendations For Future Treatment.
The purpose of a treatment plan is to understand our client’s areas of struggle, and to collaboratively guide patients towards their mental health goals. Web a treatment summary documents a client's progress and health over a period of time, allowing you to see the overall effectiveness of treatment. Treatment plans are an effective tool for improving patient engagement in their treatment because they outline their current struggles and how they will overcome them with a therapist's help. Join thousands of happy therapists using mentalyc ai.
Psychological Therapies For People With Severe Mental Health Problems (Also Referred To As Severe Mental Illness) Are A Key Part Of The New Integrated Offer For Adults And Older Adults, As Set Out In The Nhs Long Term Plan (Ltp) And The Community Mental Health Framework For Adults And Older Adults.severe Mental Health.
A discharge note, also called a termination note, is a written summary held in the client’s chart of what happened during the time the client was in your care. Web a treatment plan template. 2 best forms for group counseling sessions. He didn’t have any physical limitations.
It’s typically completed within your first few sessions with a client. Counseling typically begins with the intake and the assessment process. 14/03/2024 | next review date: Web this document is a template of a mental health treatment plan. What is a case conceptualization or formulation?